Recently, significant advancements have been made in stem cell treatment for diabetes. This year, Vertex released clinical data on its continuing stem cell therapy for diabetes treatment. Two patients with type I diabetes, who underwent stem cell therapy for over a year, no longer require insulin injections, and have shown remarkable improvements in their diabetes-related symptoms and biochemical indicators. Today, we will discuss the effectiveness and obstacles of stem cell treatment for diabetes based on literature reports, aiming to enhance everyone’s understanding of this innovative approach.
Recently, Vertex Pharmaceuticals (VRTX.US) announced the latest data from the phase 1/2 clinical trial of its diabetes stem cell therapy VX-880 at the American Diabetes Association Annual Scientific Meeting (ADA): More than a year later, the two patients with type I diabetes no longer need insulin injections, and their diabetes-related symptoms and biochemical indicators have been significantly improved.
This is a Phase 1/2, multicenter, single-arm, open-label study in patients with type 1 diabetes (T1D), demonstrating the potential of stem cell-derived islet cell therapy as a future treatment option for patients with type 1 diabetes.
This study focused on adults with type I diabetes who had impaired hypoglycemia awareness and severe hypoglycemia. All six patients treated with VX-880 had undetectable insulin secretion and recurrent severe hypoglycemia in the year prior to treatment. History of the incident.
After treatment, all patients showed restoration of insulin secretion, improved glycemic control, reduction or elimination of exogenous insulin use, and a complete absence of severe hypoglycemic events during the 90-day evaluation period, the ADA said.
“These new findings demonstrate the potential of stem cell-derived islets as a future treatment for patients with type 1 diabetes and mark a new era that may eliminate the need for external source of insulin to achieve glycemic control.”
Currently, this research has been extended to Norway, Switzerland and the Netherlands. Further data on this therapy are still worth looking forward to.
Diabetes: nearly 600 million patients worldwide, it is urgent to explore new treatments
Diabetes is a multifactorial metabolic chronic disease characterized by chronic elevation of blood glucose caused by disorders of insulin secretion or function. Diabetes can cause serious complications in most systems and organs of the body, leading to disability, paralysis, and even death. The current treatment options for diabetes are mainly diet control, drug treatment or insulin treatment. These treatments cannot achieve a curative effect and may also have some side effects. In addition, the treatment of diabetes complications imposes a heavy economic burden on society.
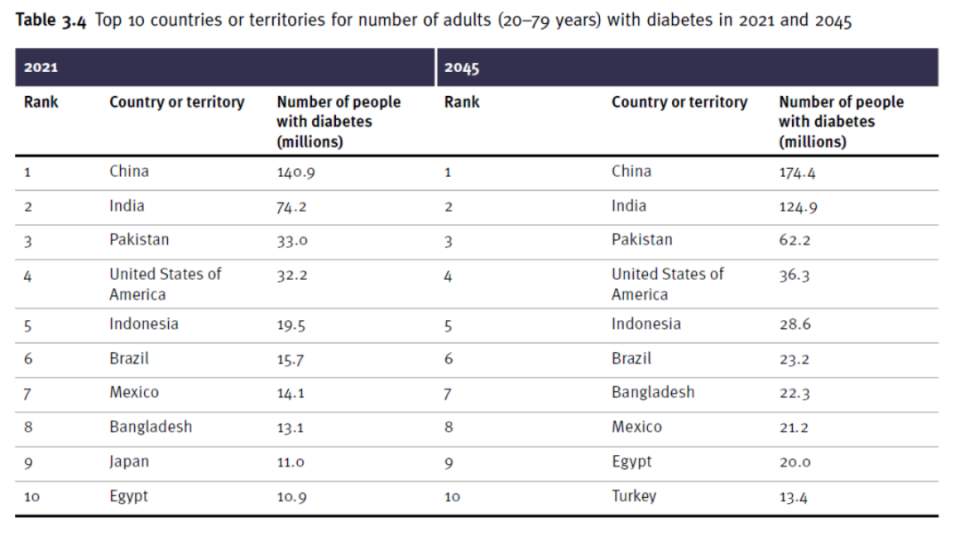
Top 10 countries or regions with the number of adults with diabetes in 2021 and 2045 (Source: “2021 IDF Global Diabetes Map (10th Edition)”)
A recent study published in The Lancet [3] pointed out that there are currently 529 million diabetic patients in the world, and this number is expected to grow to 1.3 billion by 2050. The “Diabetes Atlas (10th Edition)” released by the World Health Organization in 2021 shows that China is the country with the largest number of adult patients with diabetes. The number of people with diabetes in China in 2021 is about 140 million, and it is expected to reach 174 million in 2045. This suggests that there is an urgent need to explore suitable alternative treatments.
The efficacy and progress of stem cell therapy in treating diabetes
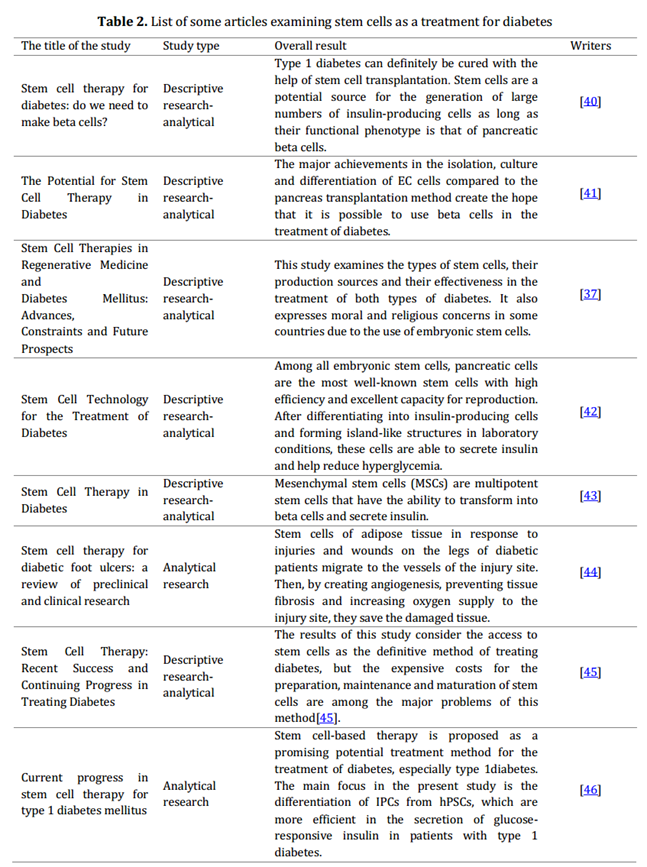
Stem cells are a renewable source of cells considered an alternative to organ transplants, with their ability to divide and transform into highly differentiated cells to replace injured and dead cells. Most scientists have long considered the possibility of using stem cells to treat diabetes and create insulin islets, which could be a hope for controlling diabetes in the future. The table lists some studies on the role, challenges and progress of stem cells in diabetes treatment [2].
Here are several clinical efficacy cases of stem cell treatment for diabetes:
Stem cells help patients with type 1 diabetes become insulin-free [4]: This study enrolled a total of 53 participants, 33 with adult-onset and 20 with adolescent-onset type 1 diabetes (T1D).
Divided into stem cell treatment group and mesenchymal stem cell treatment group, this group was followed up for 1 year after intervention. It was found that 40.7% of the subjects in the mesenchymal stem cell treatment group had significant relief of clinical symptoms, and 3 subjects maintained their symptoms for 3 to 12 months. Insulin-free state, which was not present in the control group.
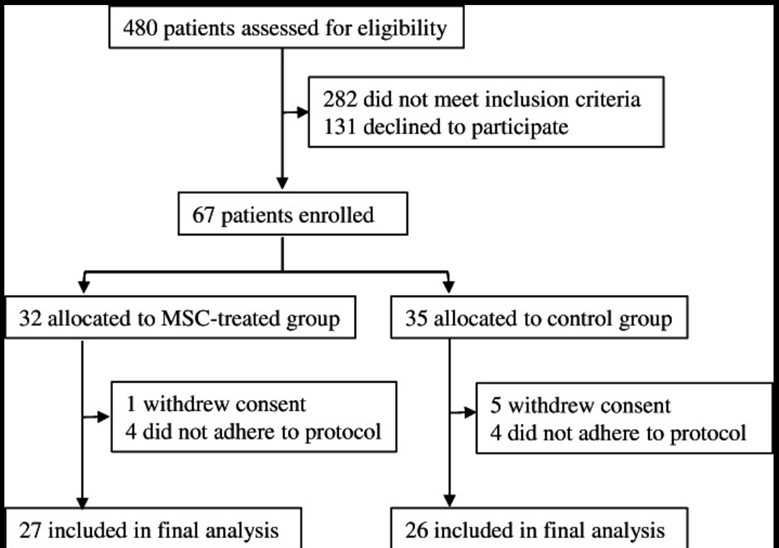
In adult-onset T1D, the percentage change in postprandial C-peptide levels was significantly higher in the mesenchymal stem cell-treated group than in the control group. The above follow-up results show the significant efficacy of stem cells in treating T1D, and no serious side effects were observed during treatment and follow-up.
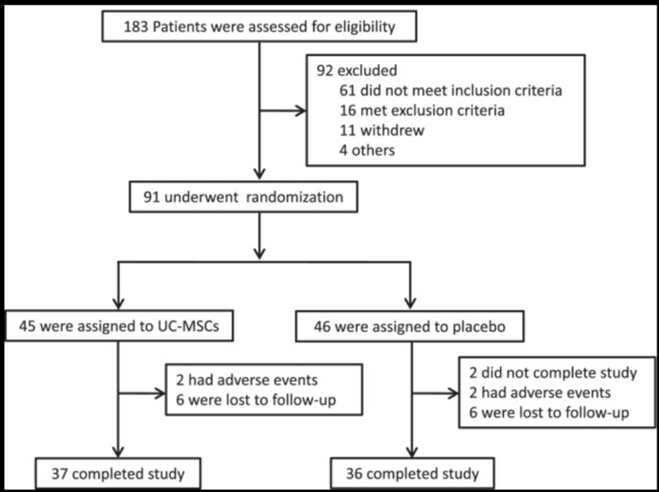
Stem cell treatment of type 2 diabetes [5]: Chinese researchers published the results of a phase II clinical trial on the efficacy and safety of mesenchymal stem cells in the treatment of type 2 diabetes in Chinese adults in the journal Stem Cell Research & Therapy. This study included a total of 91 patients with type 2 diabetes (T2D), who were divided into a mesenchymal stem cell treatment group and a placebo group, and were followed up for 48 weeks.
The results found that 20% of patients in the mesenchymal stem cell treatment group had glycated hemoglobin (HbA1c) levels <7.0%, and the daily insulin dosage was reduced by more than half. In addition, the mesenchymal stem cell treatment group’s HbA1c level decreased by 1.31%.
Compared with the placebo group, only 4.55% of patients in the placebo group achieved HbA1c <7.0%, and the overall HbA1c only decreased by 0.63%. In summary, mesenchymal stem cell therapy significantly improved T2D, and there were no related adverse reactions during treatment and follow-up.
Stem cell treatment of diabetic foot ulcers [6]: Studies have shown that adipose tissue stem cells migrate to blood vessels at the site of leg injuries and wounds in diabetic patients, and then have multiple effects such as creating angiogenesis, preventing tissue fibrosis and increasing oxygen supply to the injured site. To repair tissue and thereby repair diabetic foot ulcers.
Challenges faced by stem cells in treating diabetes: The above data allow us to see the hope of stem cells in treating diabetes and provide an ideal treatment method for diabetic patients. However, when reaping the therapeutic effects, we also need to face up to the challenges brought by stem cell therapy.
These challenges include:
- Improving the functions of produced stem cells to prevent excessive proliferation and potential teratoma formation, while ensuring proper differentiation and functionality, such as insulin secretion in derived islet cells.
- Addressing immune rejection, reducing stress reactions, and enhancing graft survival rates post-transplantation.
- Resolving ethical issues related to stem cell therapy and pursuing further advancements.
Summary
To sum up, stem cells, as an emerging disease treatment method, also show great potential in treating diabetes. Although the use of stem cell replacement methods to treat diabetes faces many challenges, I believe that with the continuous improvement of technology, in the future development, a cure for diabetes will no longer be out of reach.
References:
- https://www.statnews.com/2023/06/23/vertex-diabetes-cell-therapy-insulin/
- Farzaneh Fazeli; Masumeh Ahanjan. “The capacity of stem cells in treatment of diabetes”.Cellular, Molecular and Biomedical Reports, 2, 4, 2022, 230-244. doi: 10.55705/cmbr.2022.357066.1060
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023 Jul 15;402(10397):203-234. doi: 10.1016/S0140-6736(23)01301-6. Epub 2023 Jun 22. Erratum in: Lancet. 2023 Sep 30;402(10408):1132.
- Lu J, Shen SM, Ling Q, Wang B, Li LR, Zhang W, Qu DD, Bi Y, Zhu DL. One repeated transplantation of allogeneic umbilical cord mesenchymal stromal cells in type 1 diabetes: an open parallel controlled clinical study. Stem Cell Res Ther. 2021 Jun 10;12(1):340. doi: 10.1186/s13287-021-02417-
- Li Zang, et al. Efficacy and safety of umbilical cord derived mesenchymal stem cells in Chinese adults with type 2 diabetes: a single center, double blinded, randomized, placebo controlled phase II trial. Stem Cell Res Ther. 2022, 13 (1):180.
- Lopes L, Setia O, Aurshina A, Liu S, Hu H, Isaji T, Liu H, Wang T, Ono S, Guo X (2018) Stem cell therapy for diabetic foot ulcers: a review of preclinical and clinical research. Stem cell research & therapy 9 (1): 1-16.